Health and social care work can be hugely rewarding, but it’s also an industry in which the stakes are high in terms of health and safety. It’s about settings that involve vulnerable people—children, older people, and people with physical or mental health issues—so ensuring high safety standards is not just a matter of complying with the law; it’s a matter of morality.
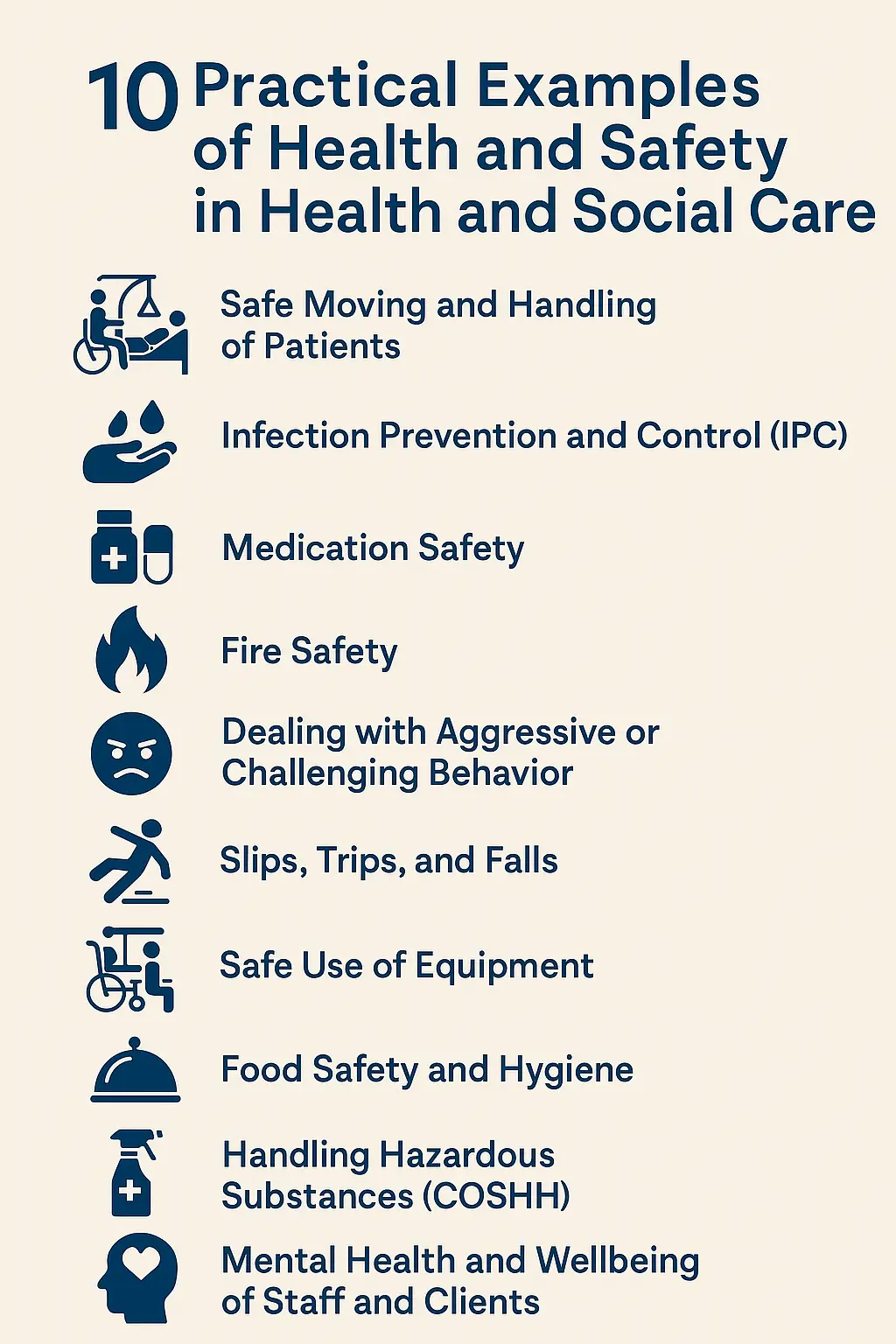
Today, let’s go through 10 day-to-day, real-life examples where health and safety are pertinent to your everyday role in care settings. Regardless of whether your role is caregiver, manager, cleaner, or nurse, the following examples should be part of your work on a day-to-day basis.
Examples of Health and Safety in Health and Social Care
1. Safe Moving and Handling of Patients
One of the most common causes of harm in care work is the improper lifting or moving of people. Imagine a carer trying to lift an older person from a wheelchair onto a bed without equipment or help. That’s a recipe for disaster—both for the client and the staff member.
What should be done:
Staff looking after the individual must be taught proper moving and handling. Hoists, slide sheets, or transfer boards are not just useful, they are unavoidable. Always assess each situation: Can the individual assist? Is there a risk of fall or back injury? Use two staff members if required, and never skip risk assessments.
2. Infection Prevention and Control (IPC)
Especially in the post-COVID age, IPC has gained importance. Think of a care home where staff does not wear gloves when they change dressings or fails to wash their hands between residents.
What should be done:
Hand hygiene is your friend—before and after every contact. Utilize PPE correctly: gloves, mask, and aprons. Correctly dispose of clinical waste. Clean high-touch points like door handles and bed rails regularly. Include IPC training as part of your regular refresher course, not just a box to be ticked.
3. Medication Safety
This one is enormous. Most workers are tasked with giving or assisting clients in taking medication. A mistake here is a serious injury or death.
What should be done:
Always follow the “five rights”: right person, right drug, right dose, right route, and right time. Use an MAR (Medication Administration Record) chart. Store meds safely—Controlled drugs need extra precautions. Don’t force a client who refuses a dose—document and report to the nurse or manager.
4. Fire Safety
Imagine a care home with blocked fire exits or no thought-out evacuation route. In the case of an emergency, the outcome would be catastrophic.
What should be done:
Hold regular practice fire drills. Clear paths for exit—no chairs or trolleys blocking the way. Ensure staff are trained in the use of fire extinguishers and are familiar with the evacuation procedure. Particular attention must be given to mobility-impaired residents: Are evac chairs or individual evacuation plans in place?
5. Dealing with Aggressive or Challenging Behavior
It’s not uncommon to have someone who will become violent with dementia, mental illness, or frustration. Everyone’s safety is most important.
What should be done:
Ensure the staff is conflict resolution and de-escalation trained. Remain calm, provide people with space, and avoid using aggressive body language. Report the incident each time so that the support plans can be reviewed and modified. In other situations, it may be a good idea to have someone accompany you.
6. Slips, Trips, and Falls
A slick floor, a rolling rug, or an electric cord might be a nasty tumble for a frail person. It’s easy but with severe ramifications.
What should be done:
Clear away the spill immediately and put clear “wet floor” markers. Conduct scheduled walk-throughs to check for hazards. Light all areas, and clients need to be utilizing proper footwear and mobility devices. Risk assess individuals who are most likely to have a fall risk—typically, a fall risk plan will need to be utilized.
7. Safe Use of Equipment
From oxygen cylinders to wheelchairs, hoists, there is equipment everywhere in health and social care. Faulty or poorly used equipment can injure staff or clients.
What should be done:
Inspect and maintain all equipment regularly. Train staff to use it correctly and keep user manuals on hand. Don’t do it by eye—if it’s broken, label it up and report for repair. Always check weight limits and specs.
8. Food Safety and Hygiene
Staff can frequently be exposed to food in nursing homes or supported living for vulnerable patients. Food poisoning results from poor food hygiene, and food poisoning is life-threatening to elderly or immunocompromised patients.
What should be done:
Follow food hygiene regulations strictly: wash hands before handling food, keep raw and cooked foods separate, and store food at the correct temperatures. Check use-by dates and always clean surfaces before and after preparing meals. Ideally, staff should have a basic food safety certificate.
9. Handling Hazardous Substances (COSHH)
From hospital waste to disinfectants, health and social care professionals are frequently exposed to hazardous chemicals. Unchecked, these can lead to burns, inhalation problems, or infection.
What should be done:
All the chemicals have to be labelled and stored in locked cupboards. Use COSHH data sheets and correct PPE when dealing with substances. Never mix chemicals or work with chemicals in a sealed space. Bins for clinical waste and not standard bins should be used for disposal of waste like soiled dressings.
10. Mental Health and Wellbeing of Staff and Clients
Not only is safety and health a bodily concern—it is also a state of mind. Burnout, stress, and emotional exhaustion pervade the industry, and can lead to error or even catastrophe.
What should be done:
Encourage open communication. Underperforming team members need to be able to speak up when necessary. Mental health support, regular breaks, and counseling or stress management training, for example, need to be provided by managers. Clients need to have regular well-being checks, socialization, and mental health care plans accordingly as well.
Conclusion
Safety and health in health and social care isn’t about scaring people or being difficult—it’s about creating an environment where individuals feel safe, can thrive, and receive the assistance they need. These are merely a couple of examples, but they are indicative of day-to-day, on-the-ground realities.
Here is what I tell every care team I work with:
-
Stay alert – Most accidents are preventable with a bit of extra attention.
-
Speak up – If something seems unsafe, say something. Your voice can save a life.
-
Keep learning – Health and safety is always evolving—what worked last year might not be best practice today.
Remember: You are not alone. Health and safety is everyone’s job, but it works best when you work together.
Related Posts
Environmental Health and Safety Concerns Ethics
8 Most Important Personal Hygiene Items and Their Uses
What is the Safe and Healthful Workplace Clause
What is HESMS and Applicable Governmental Regulations
A seasoned Health and Safety Consultant with over a decade of hands-on experience in Occupational Health and Safety, UBONG EDET brings unmatched expertise in health and safety management, hazard prevention, emergency response planning, and workplace risk control. With a strong passion for training and coaching, he has empowered professionals and organizations to build safer, more compliant work environments.
Certified in globally recognized programs including NEBOSH, ISO standards, and OSHA regulations, he combines technical know-how with practical strategies to drive health and safety excellence across industries. designing comprehensive HSE management systems or delivering impactful safety training, whether he] is committed to promoting a culture of safety and continuous improvement.